Connect With Us
Blog
Items filtered by date: December 2021
Symptoms and Prevention of Athlete’s Foot

Athlete's foot is a fungal infection that affects the skin on the feet, commonly caused by the fungus, trichophyton. Symptoms include itching, burning, and redness between the toes, along with peeling and cracking skin. In more severe cases, blisters and swelling may occur. Prevention is essential to avoid this uncomfortable infection. Keeping feet clean and dry is essential, as fungi thrive in moist environments. Wearing breathable, moisture-wicking socks and well-ventilated shoes helps reduce the risk. Avoiding walking barefoot in communal areas, such as locker rooms or swimming pools, can prevent exposure to the fungus. Regularly changing socks and practicing good foot hygiene further reduces the likelihood of becoming infected. Athlete’s foot can be uncomfortable and unsightly. If you have developed this fungal infection, it is suggested that you consult a podiatrist who can offer you effective treatment solutions, which may include prescribed medication.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact Leonard Talarico, DPM from Georgia. Our doctor will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our office located in Pooler, GA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How to Deal with Athlete's Foot
Athlete’s foot is a type of fungal infection that affects the skin on the feet. It is caused when the tinea fungus grows on the foot. It is possible to catch the fungus through direct contact with someone who has it or by touching a surface that is contaminated with it. This type of fungus thrives in warm, moist environments such as showers, locker room floors, and swimming pools. Your risk of getting it may also increase by wearing tight-fitting, closed-toe shoes, or by having sweaty feet.
Symptoms of athlete’s foot include itching, stinging or burning sensations between the toes. You may also experience toenails that are discolored, thick, crumbly, or toenails that pull away from the nail bed.
Your podiatrist may diagnose athlete’s foot by detecting these symptoms or by doing a skin test to see if there is a fungal infection present. The most common exam used to detect Athlete’s foot is a skin lesion potassium hydroxide exam. To use this method, your doctor will scrape off a small area of the infected skin and place it into potassium hydroxide. The potassium hydroxide will destroy the normal cells and leave the fungal cells untouched so that they are visible under a microscope.
There are a variety of treatment options for athlete’s foot. Some medications are miconazole (Desenex), terbinafine (Lamisil AT), clotrimazole (Lotrimin AF), butenafine (Lotrimin Ultra), and tolnaftate (Tinactin). While these options may be able to treat your fungus, it is best that you consult with a podiatrist in order to see which treatment option may work best for you.
In some cases, Athlete’s foot may lead to complications. A severe complication would be a secondary bacterial infection which may cause your foot to become swollen, painful, and hot.
There are ways that you can prevent athlete’s foot. Washing your feet with soap and water each day and drying them thoroughly is an effective way to prevent infections. You also shouldn’t share socks, shoes, or towels with other people. It is crucial that you wear shower sandals in public showers, around swimming pools, and in other public places. Additionally, you should make sure you wear shoes that can breathe and change your socks when your feet become sweaty. If you suspect that you have Athlete’s foot, you should seek help from a podiatrist as soon as possible.
Symptoms of Foot Stress Fractures

Foot stress fractures are tiny cracks in the bones that develop over time, often due to repetitive force or overuse, and are common to runners and other athletes. One of the main symptoms of a foot stress fracture is tenderness, where the injured bone feels painful to touch. Known as pinpoint pain, this can be accompanied by deep, dull pain that seems to originate from within the foot or toes. You may also experience weakness in the affected area, leading to reduced performance in daily activities. Intermittent pain is typical, intensifying during weight-bearing activities, like walking or running, and diminishing with rest. Swelling is another sign of stress fractures, usually visible on the top portion of the foot due to injury to a metatarsal bone. Changes in biomechanics, such as altered walking or running patterns to avoid pressure on the painful area, may also occur. Sharp, localized pain might be felt when putting weight on the foot, particularly in more severe injuries, and bruising may be present, causing reddish, bluish, or purplish discoloration. A podiatrist specializes in diagnosing and treating foot stress fractures, which can be difficult to detect through an X-ray alone. Digital imaging tests, such as an MRI scan may be required. If you believe you may have a foot stress fracture, it is suggested that you schedule an appointment with a podiatrist for an exam, diagnosis, and treatment.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact Leonard Talarico, DPM from Georgia. Our doctor can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact our office located in Pooler, GA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Stress Fractures of the Foot and Ankle
Our bones are important aspects of our body and they are constantly changing. The heavier the workload for a bone, the more likely it is that calcium will be placed in it. When a bone isn’t used often, there won’t be much calcium within it. When stress from repetitive loads prevent the bone from being able to repair itself, cracks will start to form. Stress fractures are defined as cracks in a bone that result from repetitive force, such as overuse.
The most common cause of stress fractures is a sudden increase in intensity and duration of physical activity. For example, if you begin to run long distances without working your way into doing so, you will be more likely to develop a stress fracture.
Common symptoms of stress fractures are pain and swelling near the weight bearing area on the injured bone. When initial x-rays are performed, it is possible that the fracture will not show up. However, once the stress on the area continues, the damage will increase, and the fracture will be severe enough to show up on an x-ray. Certain parts of the foot are more likely to develop stress fractures than others. Areas that typically have these fractures are: the metatarsals, the navicular bone, the calcaneus, tibia, and fibula.
Since women are at an increased risk of developing osteoporosis, they are twice as likely as men to sustain a stress fracture. Additionally, old age causes a decrease in bone mineral density which is why elderly people are also likely to develop these fractures.
It is important for you to be professionally diagnosed by a podiatrist if you suspect you have a stress fracture, because there are other injuries that can easily be mistaken for a fracture. Sprains, strains, shin splints, plantar fasciitis, and Morton’s neuroma can all easily be mistaken for stress fractures in the foot. Your podiatrist will likely ask you a series of questions to determine what type of pain you are experiencing. These questions will help your doctor identify whether you have a stress fracture.
The best method of treatment for a stress fracture is rest. Additionally, a walking boot, cast, or crutches, will help rest the area that is injured. The typical healing time for stress fractures is 4-12 weeks, however this depends on which bone is involved.
Arthritis Can Cause Pain in the Feet and Ankles
How Peripheral Artery Disease Affects the Feet
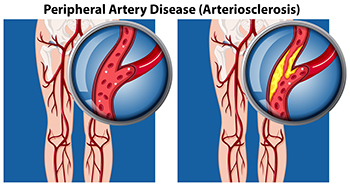
Peripheral artery disease, or PAD, affects blood circulation, often manifesting through symptoms related to the feet. Common signs include cramping, pain, or numbness in the feet during physical activity, which subsides with rest. Coldness or discoloration of the feet or toes, particularly in comparison to the unaffected leg, may also occur due to reduced blood flow. Slow-healing wounds or sores on the feet are another indicator, as PAD limits the delivery of oxygen and nutrients essential for tissue repair. PAD, caused by narrowed arteries due to plaque buildup, increases the risk of complications, such as infections and tissue death in severe cases. Regular foot exams from a podiatrist are essential for managing PAD. If you have symptoms of PAD, it is suggested that you are under the care of this type of doctor who can help you to manage this condition.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Leonard Talarico, DPM from Georgia. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in Pooler, GA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Preventive Training for Running Injuries

Preventing running injuries involves a combination of smart training techniques and maintaining overall strength. Gradually increasing mileage and intensity helps avoid overuse injuries by allowing the body to adapt to new demands. Incorporating rest days into the training schedule gives muscles time to recover and reduce fatigue. Strength training, especially for the core and lower body, enhances stability and reduces strain on joints. Proper warm-ups and cool-downs, including dynamic stretching, prepare the body for running and aid in recovery. Listening to the body and addressing any pain or discomfort promptly can prevent minor issues from becoming serious injuries. Wearing well-fitted, supportive footwear tailored to individual running styles also plays a crucial role. Foot and ankle injuries can be common and will hinder running ability. If you have sudden or chronic foot pain from running, it is suggested that you contact a podiatrist who can offer you effective treatment and running prevention injury methods.
Exercising your feet regularly with the proper foot wear is a great way to prevent injuries. If you have any concerns about your feet, contact Leonard Talarico, DPM of Georgia. Our doctor will treat your foot and ankle needs.
How to Prevent Running Injuries
Many common running injuries are caused by overuse and overtraining. When the back of the kneecap starts wearing out and starts causing pain in your knee, this is commonly referred to as runner’s knee. Runner’s knee is a decrease in strength in your quadriceps and can occur if you’re not wearing properly fitted or supporting shoes. To prevent runner’s knee, focusing on hip strengthening is a good idea, as well as strengthening your quads to keep the kneecaps aligned.
What Are Some Causes of Running Injuries?
- One cause of a common running injury is called iliotibial band syndrome.
- Plantar fasciitis is also another common injury.
- Stress fractures can occur from overtraining, lack of calcium, or even your running style.
Best Ways to Prevent Running Injuries
- Wear footwear that fits properly and suits your running needs.
- Running shoes are the only protective gear that runners have to safeguard them from injury.
- Make a training schedule. Adding strengthening exercises as well as regular stretching can help keep you strong and limber and can lessen the possibility of injuries.
- Stretching keeps muscles limber; this will help you gain better flexibility.
If you have any questions please feel free to contact our office located in Pooler, GA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Preventing Running Injuries
Over half of all runners encounter at least one injury per year. The reason for this is because many runners do not train properly. Injuries are almost inevitable due to the physical stress that running causes. While our bodies are great at adapting to the stress, it can only handle it in small doses. Injuries occur when the stress is applied too quickly for the body to handle, causing something within it to break down. With each step you take, your leg is absorbing two or three times your body’s weight.
Some of the most popular running injuries are shin splints, plantar fasciitis, Achilles tendinitis, and stress fractures. Shin splints cause pain along the inside or outside of the shins, and this pain is usually felt at the beginning of a run. The condition itself is defined as an inflammation of the muscles or tendons located around the shinbone. To treat shin splints, it is advised that you ice the shin area and stretch the calf muscles. To prevent this injury, you should slowly increase the distance you plan on running, instead of jumping into a more strenuous routine.
Achilles tendinitis is another common injury and it feels like pain along the back of the leg, toward the heel. This condition is defined as an inflammation of the Achilles which is the largest tendon in the body. The Achilles is responsible for connecting your calf muscles to the heel bone and it is caused by tight calf muscles. If you want to treat this injury, you should take a break from running to cross train with a low-impact activity.
There are a lot of common mistakes runners make that are causing them to experience injury. One mistake is stretching too much prior to warming up. If you plan to go on a run, you should warm up with a gentle 3-5-minute walk followed by a 5-minute run-walk. Another common mistake is jumping into a routine too quickly. Consequently, you should incorporate cross-training into your routine. If you are looking to get active, you should slowly weave running into an activity you are currently participating in. For example, you can try bike riding for 40 minutes followed by a 10-minute run.
Another way to prevent running injuries is to choose shoes that are appropriate for running. There are certain things you should look for when buying a new pair of running shoes. An important factor in these sneakers is flexibility. Running shoes should be capable of bending and flexing at the forefoot. However, you should not be able to bend the entire shoe in half with ease because this is a sign that the shoe does not have enough structure. Additionally, you should look for the fit of the running shoes you want to purchase. It is best to visit a specialty running shoe store to have your feet properly sized. Choosing shoes that fit properly can prevent many foot ailments.
If you are suffering from any pain from running injuries, you should make an appointment with your podiatrist to discover the underlying cause of your pain. He or she will be able to help treat your condition in the best way possible.
Causes and Treatment of Plantar Fasciitis

Plantar fasciitis, or inflammation of the plantar fascia, often leads to heel pain. This condition affects approximately 10 percent of the population at some point, with a higher prevalence in women and individuals between 40 and 60 years old. The plantar fascia is a thick band of tissue that runs from the heel to the toes. It supports the foot's arch and absorbs shock. Plantar fasciitis is considered an overuse injury. It is caused by standing for long periods, engaging in high-impact sports, or wearing poorly supportive shoes. These actions can cause microtears in the tissue, resulting in inflammation and pain. Key treatment strategies include resting the feet, avoiding activities that contribute to the pain, and taking pain relievers. Stretching exercises for the calf muscles and plantar fascia, often recommended by a podiatrist, can enhance recovery by improving strength and flexibility. Custom orthotic inserts may also provide additional support and comfort. If you are experiencing heel pain, it is suggested that you schedule an appointment with a podiatrist for an exam and treatment options.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Leonard Talarico, DPM from Georgia. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our office located in Pooler, GA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blog Archives
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
